We are living in a climate emergency. Earth’s temperature has been rising since 1880 however since 1981 warming has doubled, with 2021 the 6th warmest year on record.1 This warming is already resulting in humanitarian crises and droughts that can in turn result in conflict and mass migration particularly in the most vulnerable countries.2 The health sector is responsible for 5.2% of emissions globally.3 The World Health Organisation COP26 summate launched their Health Programme which commits signatories to develop low carbon healthcare systems with the aim to keep rising global temperatures within set limits.3 Supply chains account for the greatest proportion of emissions and are notoriously hard to control.3 Disinfectants are rarely mentioned in sustainability initiatives however are key supply chain components for healthcare systems globally. The COVID-19 pandemic has disrupted attempts to reach these goals, particularly in the healthcare setting, and increased plastic and disinfectant use has occurred.4 There has been increasing focus on evaluating the impact of, and changing healthcare practices, to avoid single use instruments, drapes and PPE.4 However, disinfection, which is integral to every aspect of healthcare, from tertiary to community care has not been as robustly evaluated. Disinfectants present their own sustainability issues, from toxic degradation products to reliance on single use containers. This viewpoint highlights such issues in several commonly used disinfectants with the aim of increasing awareness of the issue and providing some potential solutions.
Use in the NHS
In NHS England medicines/chemicals (including disinfectants) and other supply chain components excluding equipment total 44% emissions.4 The NHS is responsible for ~4% of the UK’s carbon footprint4 so this figure is substantial not only for hospitals but on a national basis. In one NHS trust in March 2020 there was a 70% rise in apron/gown procurement5 which is likely reflected across trusts during the pandemic. There is extremely limited data on emissions across the disinfection industry. Disinfectants now play a heightened role due to the pandemic and sustainable alternatives will be important for green recovery. From their manufacture to their degradation products, to the consequences of transporting large volumes of liquid across continents, a unique environmental impact can be anticipated. Notably, medical ethanol production for disinfection increased 12.3% during the first year of the pandemic.6 Additionally, according to procurement data, NHS Lothian used 654200 chlorine tabs alone (not including wipes, granules or other disinfectants) in a 12-month period, highlighting again the importance of disinfection products and the potential sustainability challenges they pose.
Disinfectants globally
The health sector contributes 5.2% of global emissions.3 While the NHS has been working to reduce healthcare related emissions, in low and middle income countries (LMICs) healthcare related emissions have risen as services increase spending.3 In regard to disinfection in LMICs, data is sparse, however low resourced hospitals face significant challenges in maintaining hygiene. A recent trial notes the reliance upon sodium hypochlorite (bleach) poses a potential threat as there is limited staff safety and usage training.7 Supply chains of hypochlorite can also be unreliable and the products themselves inconsistent in potency.7 They note that local sourcing of disinfecting materials would improve reliance on potentially degraded and ineffective materials, improving subsequent hygiene. Producing materials on site in addition to reducing dependence on supply chains also has the benefit of reducing transport and packaging emissions, improving hospital emissions. Sodium hypochlorite also carries several hazard warnings, discussed below.
Sodium hypochlorite
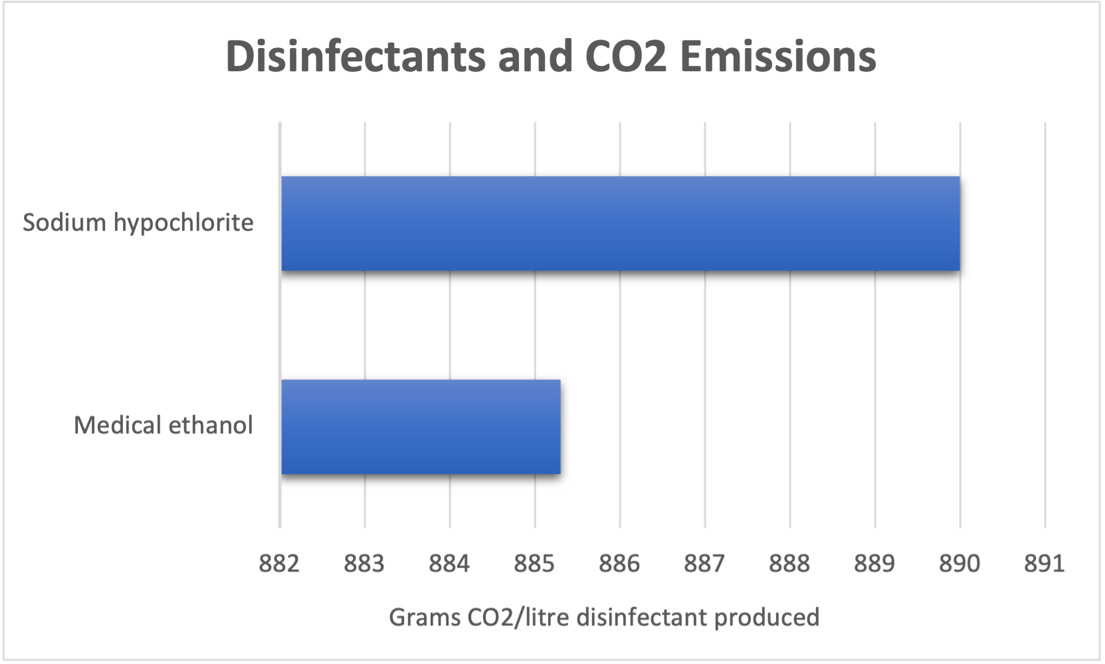
Sustainability considerations should include degradation/breakdown or disposal implications of the product. Disinfectants used in hospitals are often accompanied with warnings, i.e. toxic to aquatic life, often due to degradation products. Sodium hypochlorite is labelled as corrosive and an environmental hazard on PubChem.8 Of particular importance it carries the label, ‘very toxic to aquatic life.’ This includes a biocidal effect on both freshwater and marine organisms such as fish and algae, key components of the ecosystem.9 Long term effects on marine life have also been observed including of cyto- and genotoxicity.9 This is in part due to effects of degradation products such as AOX (chlorinated by-products) which are found abundantly in hospital effluent.10 Although usually present in safe quantities, disinfection by-products have been linked to carcinogenicity and other adverse health outcomes in humans and animals.11 Moreover, the rigour of monitoring of effluent and drinking water quality varies. This is worth keeping in mind with increased use of disinfectants following the COVID-19 pandemic, with sales of surface disinfectant predicted to rise to $9.52billion by 2029 according to analysts.12 Sodium hypochlorite has been noted to produce nearly 900g CO2/litre13 which is the around the same volume produced by a Toyota Yaris travelling 7km14 (Figure 1).
Medical ethanol
Beyond chlorine, medical ethanol use for disinfection has increased due to COVID-19, one study noting 20% growth in use of medical ethanol in 2020 (compared to an average growth of 7.7% from 2015-2019).6 Production of ethanol is associated with significant carbon emissions. One study noted production of 885.3g CO2eq/L medical ethanol,6 comparable to bleach (Figure 1).
This is particularly relevant to surgeons, as alcohol hand-rub based scrubbing increases in popularity. Beyond emissions, it is notable that antimicrobial resistance to alcohol is increasing15 – increased rates of resistance will lead to more patients requiring side rooms and increased PPE, contributing to both plastic and chemical pollution as well as increased demand on health services already coping with the aftermath of a pandemic.
Benzalkonium chloride, a quaternary ammonium (quat), has been suggested as an alternative to medical ethanol hand sanitiser. Quats are currently recognised by the U.S Environmental Protection Agency against SARS-CoV-2.16 There is limited evidence of skin sensitisation and no safety and hazard data on PubChem.17 Additionally, benzalkonium chloride can be laboratory made. This means that on site provision could be achieved, reducing both the transport emissions and single use plastics which medical ethanol hand sanitiser products are dependent on.
Chlorhexidine
Chlorhexidine is another commonly used antimicrobial in surgical theatres. It is an environmental hazard, very toxic to aquatic life and is non-biodegradable.18 One producer supplies 150000 antiseptic products a day to customers, implicating large volumes of plastic waste and associated transport emissions.19 No data on emissions from production could be sourced however several companies supplying chlorhexidine products to the NHS have sustainability goals and Net Zero targets.19 A call for increased transparency from companies on sustainability measures, including emissions data, is key to moving toward Net Zero. Several employers including the NHS have set deadlines for suppliers to provide such data. This works to ensure that all scopes of emissions are tackled and not those under direct control of the procuring organisation.
Human Factors
Human outcomes should be carefully considered in sustainability approaches. Most professional cleaning products are a mixture of substances with varying safety and ecological profiles. These mixtures have a strong association with irritant contact dermatitis of poor prognosis and may necessitate job restructuring in domestic workers in severe cases.20 Increased rates of irritant dermatitis have been reported as a result of the COVID-19 pandemic and this should be considered not only in occupational health discussions but also in sustainability strategies.21 Benzalkonium chloride has fewer reported skin sensitising issues than medical ethanol and could be an alternative for healthcare providers.17 Use of occlusive gloves also places healthcare workers at risk of hand disease therefore it is important to find alternatives that are less irritant and safe for repeated use while maintaining ease of use and acceptability.
Hypochlorous acid and redistributed manufacturing
Controlling the lifecycle and content of disinfectant products in the supply chain is extremely difficult, as highlighted here. Liquid disinfectants are relatively heavier than many other healthcare supplies that are routinely used in large volumes. Thus, adding to the carbon footprint required to package and transport them. Other industries, for example agri-food, focus on local production to decrease their carbon footprint. Redistributed manufacturing (production of materials on site), should be considered to combat this. This would reduce transport emissions and container re-use could minimise plastic waste. On site production near the point of healthcare delivery may not (yet) be possible for many products used in healthcare. Importantly, in contrast, it is possible to produce an effective disinfectant on site. Hypochlorous acid (HOCl), a potent disinfecting chlorine solution,22 can be produced by electrolysis of a solution of salt in water and does not carry aquatic or human toxicity warnings.23 This gives it potential as not only an environmental but also a humanitarian aid, important when considering that tackling climate change must be fair and sustainable development goals should co-exist. Being able to produce it on site means that substantial transport emissions of bottling and delivering other disinfection products is removed, and local water and salt sourcing can be carried out. The limited data available also suggests reduced carbon emissions compared to standard products with around 1.8grams CO2 produced per litre HOCl (nearly 500x less than sodium hypochlorite)24 (Figure 1). Hypochlorous acid has not been traditionally used in the NHS or USA however it is used in veterinary medicine and widely across the food and agriculture industry. Interesting, HOCl has been suggested for use in low resourced hospitals in Nigeria, particularly because formal hygiene training is not necessarily required for its use (as dilution is not required) and cheaper associated costs.7 They note some hospitals are now producing sodium hypochlorite locally but if a safer and easier to use product could replace this it would be of great benefit, particularly as solar energy can be used to produce electrochemically generated HOCl.7 Some manufacturers offer to supply bottled HOCl, however, this will not address the carbon cost of packaging and transport.
CONCLUSIONS
We need better clarity on the environmental impact of disinfectants, to guide informed decisions about changes to clinical practice and supply chains. As companies work towards net zero targets, we may see a rise in industry information. However, awareness of disinfectants as a sustainability issue for the NHS must increase if we are to work to improving their ecological and environmental impact. The COVID-19 pandemic has impacted work towards Net Zero but the human health implications of climate change, including childhood asthma, pollution driven health inequalities and humanitarian crises,2,4 cannot be placed second to this any longer. Disinfection is a key aspect of sustainability and should be considered in Net Zero approaches. Hypochlorous acid is a safe and effective alternative which has potential to reduce transport and packaging emissions, has improved biodegradability profile and can be generated using sustainable energy sources. Benzalkonium chloride can also be made on site and is another option if healthcare networks aim to reduce dependence on supply chains which also reducing packaging/transport associated emissions. This article provides a basis of the environmental sustainability issues incurred from disinfection, an often forgotten but key source of emissions and suggests some potential alternative routes.
Disclaimer
There are no disclaimers.
Funding
There are no funding disclosures.
Authorship contributions
KMH wrote the initial draft of the manuscript and edited the final version. FVM proposed the idea for the manuscript and edited the final draft.
Disclosure of interest
The authors completed the ICMJE Disclosure of Interest Form (available upon request from the corresponding author) and disclose no relevant interests.
Correspondence to:
Kate Homyer
NHS Lothian
Scotland
[email protected]