Anemia affects 27% of the world’s population, about 1.93 billion people. Developing countries bear a disproportionate burden of 89% of all anemia-related disability, iron deficiency being a major reason (>60%).1 Women and children (about 800 million), especially from developing countries, bear the major burden.2 Iron deficiency not only results in negative health outcomes such as increased mortality and morbidity related to maternal and child health, but also has broader societal implications like decreased cognition in children from infancy through adolescence, and reduced work productivity in adults.3 About 42% of anemia in children and 50% in women is attributed to iron deficiency and could be eliminated or reduced by iron supplementation.4 However, challenges such as poor ante-natal care-seeking, insufficient doses, or behavioral challenges to regular use have limited the effectiveness of supplementation programs. Food fortification interventions are an effective mechanism to scale-up the coverage of micronutrients and contribute to addressing gender and income-related inequities in health status. They can cost-effectively reach larger populations and are generally more socially acceptable than pharmacological supplementation, or require less effort in changing nutrition-related behaviors.5,6 India has successfully reduced the burden of iodine-deficiency disorders by legislating fortification of salt with iodine and has built an extensive infrastructure for the production and distribution of iodized salt. With minimal additions to this infrastructure, salt fortification has the potential to act as a vehicle for the inclusion of other micronutrients (such as iron) and make a similar impact on deficiencies in these micronutrients, however, only if adequately scaled-up. There is empirical evidence to support the efficacy of double fortified salt (DFS) in improving iron status and reducing the prevalence of anemia. In one such study among school children in rural southern India, the prevalence of anemia decreased from 15.1% to 5% (a drop of more than 50%).7 Another Randomized Controlled Trial among women tea pickers in West Bengal found that the intervention group using DFS had greater increase in hemoglobin (+2.4 gm/L) and body iron (+1.43 mg/kg), in comparison to the control group.8
In recent years, India has witnessed a surge in the use of fortified foods both in the public and private markets, with an intention to increase intake of essential micronutrients by large populations, which are mostly deficient as a result of poor diets. Government of India policies are reinforcing the use of fortified foods in food security programs such as the mid-day meal (MDM), Integrated Child Development Services (ICDS), and the public distribution system (PDS).9–11 The PDS is a pan-India government programme for distributing foodgrains and other essential commodities at highly subsidized prices to families pre-identified as poor and vulnerable. It operates a network of more than 500,000 fair price shops (FPS) spread across India, enabling access to more than two-thirds of the country’s population.12 These shops are owned by small local entrepreneurs who facilitate the retail distribution of subsidized food and kerosene (cooking fuel) to pre-identified beneficiaries, in exchange for a small commission. In 2015, the University of Toronto (UofT), International Development Research Centre (IDRC), Global Affairs Canada (GAC), the Tata Trusts – an Indian philanthropic organization, and the State Government of Uttar Pradesh (GoUP), collaborated to launch the rollout of encapsulated ferrous fumarate DFS through the PDS. Launched as a pilot project in ten districts of Uttar Pradesh, the project also tested the scalability of the model of distributing DFS through the Public Distribution System and its effectiveness. The specific objectives of this case study are to describe the scale-up model utilizing the PDS, assess its scalability, critically analyze the process of scaling-up, and provide evidence to shape a national DFS scale-up agenda.
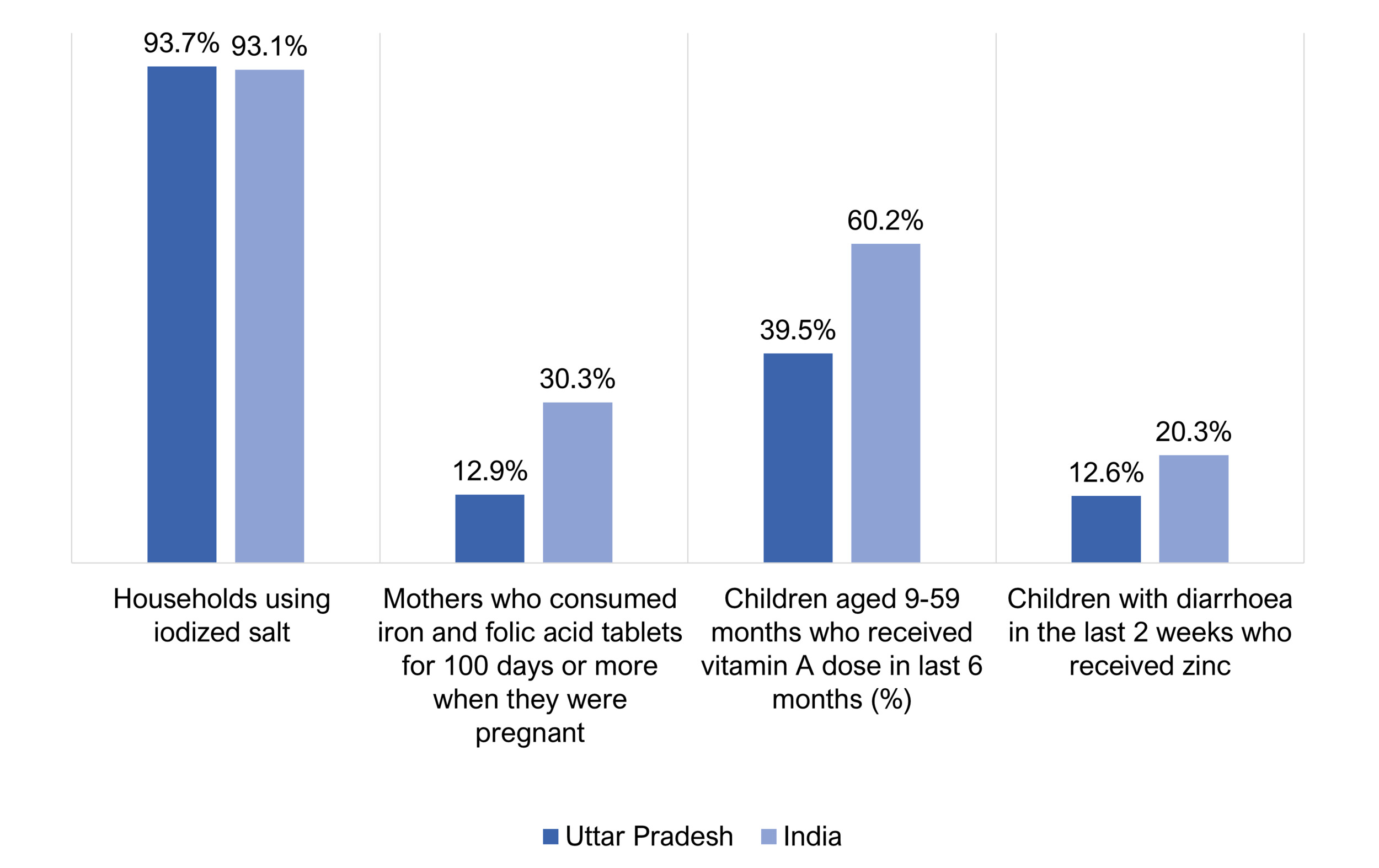
The state of Uttar Pradesh is home to a population of more than 200 million, i.e, 16% of India’s population.13 Uttar Pradesh has a high maternal mortality ratio,14 high infant mortality rate,15 a high percentage of stunted children,16 inadequate dietary diversity among children,16 and relatively high rates of poverty.17 Current efforts to address IDA are inadequate, for instance, only 12% of the pregnant women had consumed the recommended doses of 100 Iron and Folic Acid (IFA) tablets as per national guidelines,16 made freely available to the pregnant women through the facility and community-based health services of the government. The coverage of other essential micronutrient supplementation programs (except iodine through salt fortification) is also less than satisfactory (Figure 1). The introduction of DFS in an accessible and affordable manner in these settings, therefore, has a great potential to enhance iron intake on a consistent basis and reduce the high prevalence of iron deficiency anemia—a burden shared by most Indian states.
METHODS
The intervention
The UP-DFS project resulted from a unique partnership between international donors, universities, Indian private salt and premix manufacturers, a leading national philanthropic organization, and the Government of Uttar Pradesh.19 Involving the private sector was essential to provide the infrastructure to produce iron premix and DFS, and because salt production is mostly limited to the private sector. Previous efforts at introducing DFS had faced acceptability challenges primarily relating to organoleptic issues. The encapsulated ferrous fumarate formulation overcame this barrier by protecting the iron premix molecules with an inert coating agent followed by a waterproofing agent. The encapsulant would break either when the salt was used in cooking foods at high temperatures or in low pH in the gastrointestinal tract. This provides stability to the iron premix and prevents unwarranted reactions with the iodine or other contaminants present on the surface of the salt particles.20 The technology for the encapsulated ferrous fumarate iron premix was developed at UofT and transferred free of cost to JVS Foods, a private premix manufacturer in India, enabling local production of encapsulated DFS in India. The construction of a full-scale commercial premix plant at JVS Foods was supported with funding from the IDRC, Global Affairs Canada (through the Canadian International Food Security Research Fund - CIFSRF), and Tata Trusts. The Tata Trusts through a subsidiary trust—The India Nutrition Initiative—provided program implementation, promotion, and monitoring support to the government of Uttar Pradesh in ten project districts. On a parallel track, the Global Alliance for Improved Nutrition (GAIN) with funding support from the Bill and Melinda Gates Foundation agreed to conduct an effectiveness trial in the ten pilot districts to assess the impact on health and nutrition status following 12 months of a continuous intervention (Table 1).
The UP-DFS scaling-up project follows the success of the salt iodization program that was built over the past 25 years and now enables access to iodized salt for 93% of the population in the country.18 A sensory trial preceding the implementation was conducted by the Department of Food and Nutrition, Institute of Home Economics, University of Delhi. The study reported 52.8% of the participants in the DFS group and 77.3% in the Iodized Salt (IS) group found no difference in the cooked dishes as compared to their usually consumed salt brand. Among those who observed a difference, 13.2% in the DFS group reported a slight discoloration, 1.9% a poorer taste, and 17% some grittiness in a few food items. Based on the convincing findings from efficacy studies and sensory trial of the encapsulated ferrous fumarate DFS, the Government of Uttar Pradesh initiated the UP-DFS project in April 2016, as a flagship program of the state government in 10 pilot districts, with a potential coverage of 15 million people. Uttar Pradesh was the first state to roll-out encapsulated ferrous fumarate DFS and one of the first two states to introduce DFS in the PDS. The program was institutionalized after a cabinet-level decision taken after dialogues and commitment from the highest levels of the government. A financial commitment of INR 480 million (approx. US$ 7 million) was made by the government of Uttar Pradesh for the provision of DFS, to the targeted population, at subsidized prices for a period of one year. The DFS manufacturer was selected by the state government through a competitive bidding process to supply the DFS. Tata Trusts provided the salt supplier with free technical assistance and technology to install facilities for the blending of premix with iodized salt, at the salt manufacturers’ factory premises. The salt supplier directly purchased the premix from the premix manufacturer.
The DFS supplier received a monthly requisition for specified quantities of DFS to be supplied to the project districts based on the number of active cardholders (registered with the PDS in the project districts). The salt-vendor supplied DFS stocks directly to government warehouses at the block level in each district (there are on average 10 blocks in each district, and within each block, there are approximately 100 fair price shops). The fair price shop owner procured the allotted quantities of DFS along with other commodities every month from block warehouses (following a pre-payment for the supplies through an e-challan system generated by the Department of Food and Civil Supplies (FCS), GoUP). The FPS owner then sold DFS bundled with other commodities at a highly subsidized price, every month, to the beneficiaries registered at his/her shop, as per their quota calculated based on the number of family members within each household. An incentive by the government to the local shopkeepers to distribute subsidized DFS to the beneficiaries was included in the original design but not implemented due to bureaucratic procedures. Rigorous quality assurance processes were followed by regular laboratory testing of salt quality and nutrient levels, both at the manufacturing end (by DFS supplier) and at receiving end (by The India Nutrition Initiative). Community Health Workers and Fair Price Shopkeepers were trained on anemia and DFS for product promotion among the community. Information panels were installed at the shops to inform the consumers on the availability and pricing of DFS. The assumptions were that regular supply of highly subsidized DFS would lead to regular purchase and utilization of DFS by the beneficiaries of the PDS system, resulting in increased iron-intake (at least 30-40% of Dietary Reference Intakes (DRI)) and decreased Iron Deficiency Anemia in the state (Figure 2).
The case study approach
This case study critically evaluates the field implementation and rollout of DFS and its effectiveness through a scalability lens. Two scaling-up frameworks from scale-up literature provide the methodological rigor to our paper and are used for synthesizing and organizing the findings of this case study. The “scalability considerations” framework21 by Milat et al. 2012, is used for scalability assessment of the UP-DFS model. The framework of “drivers” and “spaces”22 by Hartmann and Linn 2008, is used to critically evaluate the scaling-up approach, process, and scaling-up experiences and challenges. The key objective was to investigate the scalability potential of the model distributing DFS through the PDS and assess the drivers and spaces for effective scale-up. The theme of inquiry focusses on delineating the scale-up model and its pathway, scalability assessment of the model, and identifying drivers and spaces that influence the scaling-up process. The original framework of drivers and spaces identifies nine types of spaces (2 added in subsequent literature) that contribute to shaping scale-up processes.22,23 For simplicity and the purpose of this paper, we merge these spaces into three categories as policy, organizational, and fiscal (Figure S1 in Online Supplementary Document).
We use the following definitions of scaling-up and scalability to shape our understanding of scaling-up and guide our assessment of scalability of the UP-DFS project. Scaling-up is defined as “Deliberate efforts to increase the impact of successfully tested health innovations so as to benefit more people and to foster policy and program development on a lasting basis”.24 An intervention is said to be scalable if a scalable unit can be defined and if it successfully achieves nearly the same results when replicated. The scalable unit is the smallest administrative unit that includes the key infrastructural components and relationship that are likely to be encountered in the system at full scale.25 “Scalability refers to the ability of a health intervention shown to be efficacious on a small scale and/or under controlled conditions, to be expanded under real-world conditions, to reach a greater proportion of the eligible population while retaining effectiveness”.21 Another approach to scaling-up is to view it across the vertical and horizontal dimensions of the intervention. “A vertical approach involves the introduction of an intervention simultaneously across a whole system and results in institutional change through policy, regulation, financing, or health system change. A horizontal approach involves the introduction of an intervention across different sites or groups in a phased manner. These approaches are not mutually exclusive, and a combination of approaches can be used”.26 While most of our focus is on the horizontal approach to scale-up, ie, replication and expansion, we also assess the vertical scale-up processes involved in scaling-up DFS in India.
We use the case study methodology as it is most appropriate to capture implementation experiences and learnings that are difficult to capture in other evaluation approaches. Also, the first author being a part of the implementation team for the pilot and based at the field site had access to key stakeholders from policy to field who could provide insights on the processes and its complexities. The data collection methods included: i) review of program documents and monthly field-monitoring data (collected by an external agency) ii) key informant interviews with policymakers, program personnel, public and private sector stakeholders iii) field visit records and experience sharing from the field staff iv) a ballpark costing estimate of the intervention using an adapted version of the WHO method for costing of fortification interventions.27 Additionally, we use supporting statistics related to the project sourced from surveys commissioned to independent evaluators (referenced).
RESULTS
Delineating the UP-DFS scale-up model
The key components for scaling up DFS through the PDS fall into three major functional domains with each domain dominated by either public, private, or civil sector and includes their coordinated efforts. The model is graphically represented in Figure 3. The three functional domains of the model and their inter-related functions are elucidated below.
The three functional domains
i. Public sector: Government policies; technical standards and regulations; budgetary commitment; optimally functioning public distribution system.
ii. Private sector: Production and distribution of DFS
iii. Civil sector (including beneficiaries): Consumer awareness and advocacy; willingness to purchase; and purchasing capacity
The inter-related functions of the three domains
Creating an enabling policy environment for ensuring sustainable replication of the DFS intervention is the most fundamental step to the scale-up of DFS. Technical guidelines and government endorsements in the form of policy directives and advisories provide the necessary political will for the new intervention to thrive. Developing and disseminating the technical standards and regulations for DFS is critical to ensure the quality of the product and achieve the desired health goal. The second domain of DFS scale-up relates to creating a sustainable market for the production and distribution of DFS. This requires investment in technology and infrastructure from the private sector and assured markets (both public and private) for DFS and premix manufacturers. Government standards for DFS guide manufacturers on adherence to quality requirements. Regulatory authorities in the government monitor the product at different levels from production to consumption to ensure compliance with regulatory standards. Efficient and equitable distribution channels such as the public distribution system, is one of the most critical elements of scaling up DFS. The third functional domain of the scale-up model encompass creating demand for DFS through advocacy and product promotion by different civil sector groups.
Findings on the coverage, uptake, and utilization of DFS from monitoring data
On average 4000 Metric Tons (MTs) of DFS was supplied through 8500 delivery points (Fair Price Shops) to cover a population of 15 million beneficiaries, every month; a total of approx. 55, 000 MTs of DFS supply for one year. High purchase rate of DFS from the PDS shops (>90%) resulted from the ‘bundling’ of subsidized DFS with other food commodities. However, more than 80% of beneficiaries surveyed were unaware of the health benefits of DFS. About 17% had the knowledge that DFS is good for health but did not know about the benefits. Among those who purchased DFS at-least once (99%), the monthly coverage of regular DFS use for all table salt showed a decline from 63% mid-year to 51% at the year end. Overall about 56% of the respondents were using DFS for all or most food purposes (all 50% and most 6%). About 15% were using DFS irregularly in some foods or sometimes, and 29% reported to have stopped using DFS at the end of one year (non-food or animal use 12%, not using at all 17%). Major reasons for non-regular use were: DFS giving a slightly dark appearance to cooked food, premix (coated iron) particles visible in the salt (perceived as impurities), and community preference for a specific popular brand and physical appearance of salt—pure white, refined, and equal particle size (perceived to be of high quality).
Scalability of the intervention using the scalability considerations framework
The scalability considerations used for this case study are effectiveness, reach and adoption of the intervention; workforce, technical and organization resources required; cost considerations; intervention delivery; contextual factors; and appropriate evaluation approaches.21 We present a summary of the scaling-up considerations assessment below; for a detailed assessment please see Table S1 in Online Supplementary Document. The UP-DFS model meets most scaling-up considerations, especially effectiveness and reach, considering the proven efficacy of the product and pan-India expansive reach when distributed through the public distribution system. The Public distribution system reaches a majority of the poor and near-poor population and thus ensures that the most eligible populations are reached and benefited by the intervention. Using the government platforms allows to subsidize the product and make it affordable. Similar high levels of anemia prevalence in most states in India justify the national scale-up of this intervention if found effective. Salt being a universally consumed product in daily uniform quantities adds to the scalability factor of the product. Adoption of the product, however, is pushed by bundling of the DFS with other commodities and may not necessarily ensure consistent utilization. Organoleptic properties of DFS, especially the slight discoloration of cooked food, coupled with low awareness on DFS, is a major barrier to effective coverage. The model however successfully demonstrates a scalable public-private-civil sector partnership for collaborative investments in the organization and technical infrastructure for DFS production and delivery, while building-in appropriate incentives for all stakeholders. Since DFS must be consumed as regular salt no special technical expertise is required by field implementers. The additional industry cost was found to be marginal (US$ 0.17) per beneficiary per year. The program implementation cost was estimated at (US$ 0.50) per beneficiary per year (Table S2 in Online Supplementary Document). The cost is however estimated to be much lower in full scale-up, considering economies of scale. However, though the consumer is offered high-quality salt at much lower price than the market rate, continuing subsidies may be challenging for state governments in the long run. The most-significant challenges arise from acceptability of the product by consumers and lack of health awareness affecting the demand of the product.
Exploring “drivers” and “spaces” (to scale-up) of the model
Drivers of the scale-up
A driver is defined as what moves a development intervention forward on the path from inception or pilot to a larger scale.22 We explore the role of the following potential drivers in the scale-up of the DFS pilot: Ideas/Solutions, Vision of scale, Leadership/Champions, Market or Community Demand, Incentives and Accountability, and External Catalysts.22,23 The innovative solution of encapsulating iron to produce the DFS was the key driver setting the momentum to scale-up of DFS in India by considerably reducing discoloration of food cooked with DFS—the main barrier to DFS uptake. The nation-wide expansive machinery offered by the Public Distribution System was the primary reason that helped accelerate the scale-up beginning with one state and a few more following in a short time. “Leaders/Champions demonstrate persistence, have skills to form alliances and credibility to mobilize resources for the scale-up”.26 The multi-stakeholder collaboration under the UP-DFS project played a critical leadership role in nurturing the idea and its practical application in the field. The University of Toronto through funding from IDRC and Global Affairs Canada transferred the technology of encapsulation by helping set-up the first commercial scale-micro encapsulation plant in India in Jaipur, Rajasthan, in 2015 (an earlier plant using the basic encapsulation technology was set up in Pune, Maharashtra, with funding support from Micronutrient Initiative—now Nutrition International—in 2000. This plant supplied limited quantities of salt to the Mid-Day-Meal program in Tamil Nadu, India). Tata Trust – a philanthropic wing of a large corporation in India supported the implementation of the DFS scale-up in Uttar Pradesh and expanded the support to other states through its subsidiary—The India Nutrition Initiative. The Food and Civil Supplies department of the Government of Uttar Pradesh governing the PDS was the nodal agency for the project implementation and the fulcrum of the project’s success. The collective leadership of these agencies was a critical factor driving the scale-up.
The success of the scale-up, however, heavily depended on consumer/market demand and acceptability of the product. Where demand already exists scaling-up could be relatively easier, however, for an innovative product such as the DFS, demand had to be created before scaling-up. In the case of UP-DFS, this was achieved to a large extent by subsidizing DFS, bundling it with other commodities of the PDS, and making it available at the nearest delivery point. To overcome the barrier of the residual challenge of organoleptic properties of DFS, particularly color change of cooked food (as the encapsulation reduces but not eliminates the discoloration) communication and awareness campaigns were organized. The model targeted the front-line functionaries of the PDS (local shop owners) and frontline health workers in the health department (Accredited Social Health Activists (ASHAs) and Auxiliary Nurse Midwives (ANMs)) to promote DFS in their work areas.
There has been inadequate attention given to the role of consumer demand as a driver for scale-up in the UP-DFS scale-up project and is possibly a weakness of the scale-up model. However, bundling of the DFS with other commodities of the PDS kit led to a push system and increase in purchase rate of the DFS, though not ensuring consistent utilization by all buyers. The subsidy provided by the government of Uttar Pradesh was presumed to be an important driver of scale-up by making the DFS preferable in comparison to other market salts. However, many beneficiaries were unaware of the subsidy, as most shopkeepers bundled the price of individual commodities, paid as a lump-sum by the consumer. Also, findings from field visits revealed that a specific section of the population (mostly urban) continued to buy high-end market salt while some (mostly rural) continued to use loose crystal salt (along with DFS). The incentive to the fair price shop keeper was included in the original design but not implemented due to bureaucratic processes. This was a significant demotivation for many fair price shop owners who reluctantly submitted to departmental orders for participating in the intervention. However, following sensitization workshops, many shopkeepers were willing to contribute to the intervention as a social cause.
Spaces for scaling-up
The policy space
Under the policy space, we examine the policies, laws, and regulations related to fortification as a part of national nutrition policies and programs; including the relative positioning of the UP-DFS intervention. (Figure S2 in Online Supplementary Document). With an increased focus on nutrition, especially on anemia reduction, the project had been positioned in an enabling environment with a high political will to support fortification initiatives at the national level. Directives and advisories (from the Ministries of Women and Child Development, Human Resource Development, and Food and Civil Supplies) encouraged the state governments to include fortified foods in their food security programs.9–11 The Food Safety and Standards Authority of India (FSSAI) had issued regulations related to standards of fortified foods, providing clear guidance of the choice of food vehicles (including salt) and related fortificants and level of micronutrients.28 Though central government and regulatory bodies endorsed and promoted the use of fortified foods in public programs, budgetary commitments were lagging. The UP-DFS project was a state-owned initiative of the Uttar Pradesh government with subsidies and other logistic costs for DFS coming from the state budgets. DFS had to compete with other priorities of the state government for continuity and scale-up.
Organizational space
The organizational space explores the infrastructural and functional requirements that are necessary for successful scale-up. These are institutional capacity, partnerships, culture, environment, and learning.22 Multi-sectoral partnerships between the state governments, and premix and salt vendors, technical facilitation by national development organizations, and catalyst organizations such as external donors and global universities, were critical to nurture the intervention in its initial stages. As the intervention expands, state and central governments (for policy and budgetary commitments), premix and salt manufacturers (for DFS production and quality), and government regulatory bodies (for quality assurance) play a major role in expanding and sustaining the intervention. Institutional capacity for production of iron premix and DFS was a significant barrier to the initial uptake of DFS. Public policies favoring fortification took time to be implemented for lack of required infrastructure. Private manufacturers were reluctant to adopt fortification for fear of increasing production cost. However, with an increased commitment from the government and public health advocates, a few state governments took the initiative for including fortified foods in their social safety net programs. Subsequently, a large public sector market was created for DFS to which the private manufacturers quickly responded. Over the past two years, four states have introduced DFS in their PDS programs, and three premix manufacturers are in the market producing premix using the encapsulated DFS technology. More than ten salt producers have built capacity to produce DFS. Today, India has a total production capacity of approx. 2000 tons of premix per year and four salt manufacturers have introduced DFS in the private market at least in some quantities. However, only 10% of the total premix plant capacity is currently utilized and demand must catch-up with the supply potential.
Fiscal space
Fiscal and financial space assesses the financial resources and fiscal policies, including the cost-effectiveness of the intervention. These resources and policies include the market space and financial investments needed to ensure a sustained level of demand and supply, creating a sustainable market for DFS. The state government budgeted for a subsidy of INR 480 million (approx. USD 7 million) for supplying adequate quantities of DFS to 15 million beneficiaries of the PDS in ten project districts for one year. Scaling-up the project in the entire state would mean catering to a PDS beneficiary population of more than 100 million and an astronomical increase in the funding required to provide the subsidy. The initial thought process was to gradually pass on the cost of fortification (additional cost of iron fortification) to consumers. However, if prices were to increase, DFS would have to compete with other market brands that are more popular due to their physical appearance. Knowledge of DFS and its health benefits and addressing apprehensions regarding DFS due to its organoleptic properties would be critical to ensure that people buy DFS even if the prices were raised. Another constraint due to which state governments may be reluctant to introduce DFS in their beneficiary kit is that the cost of the program must be borne from the state budget as there is no central government funding for the additional cost of fortification interventions, especially the subsidy cost. DFS must, therefore, compete against other priorities of the state government for financial allocation. Another conflict is that PDS is a food security program designed to provide food items to prevent hunger and starvation. Salt does not fit the criteria and is considered a non-essential commodity in the PDS. Securing central government funds would need a policy change to designate DFS as an essential commodity of the PDS owing to the added value of being fortified with iron and iodine.
Generally, subsidies are believed to increase access.29 It was assumed in the case of UP-DFS that providing highly subsidized DFS would significantly increase its uptake and utilization. Though the subsidy should be an important consideration for poor families, it was difficult to assess its role in the actual uptake of DFS. This was because the shopkeepers sold DFS as a bundled product with other commodities and a total purchase price for the entire kit charged as a lump sum. There were efforts by the implementation team to make the consumer aware of the subsidy, such as information panels at the PDS shops. However, the process evaluation revealed that of those who purchased DFS, very few (less than 5%) mentioned reduced pricing as a reason for purchase. It should be noted that the PDS commodities are provided as an entitlement kit of a welfare scheme, leaving only two options to the consumers to buy the full package together or to forgo the benefits entirely. A ballpark costing analysis of the UP-DFS intervention suggests good financial viability based on the cost estimates (Table S2 in the Online Supplementary Document). The incremental cost of iron fortification for the salt industry is estimated to be INR 12/person/year (US$ 0.17). For the additional cost of distributing DFS through public sector channels and program implementation support INR 35/person/year (US$ 0.50) is estimated.
DISCUSSION
Scale-up models must be adaptive to accommodate the diverse socio-economic and political environment in which the scaling-up occurs. Also, scaling-up can assume different meanings in the context of different programs.22 For the UP-DFS intervention model, scaling-up means replication of the intervention to distribute/sell subsidized DFS through the public distribution system in other Indian states, i.e. horizontal scale-up. The PDS being a pan-India infrastructure offers the opportunity for national scale-up of the intervention. Another dimension to scaling-up would be the coverage of more districts within the states that have begun small by launching the intervention in pilot districts. Thus, we look at horizontal scaling-up of DFS as both replication and expansion of the UP-DFS model. Simultaneously, the intervention also attempts at vertical scale-up by influencing policy and regulations on fortification, institutional strengthening, and innovative financing mechanisms. Since the UP-DFS scale-up project was shaped by the existing policies, financing, regulation, and systems, it also influenced the vertical scaling-up of DFS by informing food fortification policies and providing ways of innovative financing for DFS scale-up through public-private and civil sector partnerships. The UP-DFS project is unique in two ways. First, it is a unique health-focused program that is implemented and managed ministry of Food and Civil Supplies that is not directly responsible for generating health outcomes. Secondly, DFS along with fortification of other food items included in the food safety-net scheme of the PDS has expanded the scope of food security programs to serve as a potential mechanism to address both macro and micro-nutrient deficiencies. The UP-DFS model builds on the ‘successful yet long’ journey of near-universal coverage of iodized salt in India. In the case of iodine, this has been mainly achieved through mandatory legislation of iodization of all salt in the market.30 The case for mandatory legislation of iron fortification, though ideal, will require more work in building evidence for impact at scale; private sector collaboration; and most importantly consumer acceptability and other ethical clearances. Meanwhile, the government food and nutrition security programs such as the Public Distribution System, Integrated Child Development Scheme, and Mid-Day-Meal in schools provide a readily available platform to reach vulnerable population especially women, children, and the low-income groups, at scale. The ICDS and MDM schemes together reach a total of over 100 million beneficiaries (pregnant and lactating women, children up to the age of 13). However, poor utilization rate of the services of both these programs,31 along with a one-time food supplementation to most beneficiaries, can considerably reduce the impact potential of DFS interventions in these programs. In contrast, the PDS delivery platform is a sustainable social-business model involving a distribution network of local shops. The delivery platform reaches 67% of the country’s population (nearly 75% of the rural population and 50% of the urban population) reaching more than 800 million individuals. The PDS system caters to households from the lower-income groups, that are most vulnerable to iron-deficient diets and anemia. The public distribution delivery mechanisms allow for subsidization of the product removing financial barriers to access. The availability of DFS at the local shops of the PDS that are frequently visited by people to collect other rations also helps to create demand by providing a nudge factor. The PDS has been criticized for leakage and pilferage of commodities, however, new monitoring systems using electronic point of sales machines, wider promotion of entitlements, a telephonic grievance reporting mechanism and such other initiatives (mostly community empowerment measures and awareness on entitlements) have considerably overcome this constraint.32
The project baseline assessment revealed that 80% of the households in the project areas utilized PDS to regularly purchase their requirements of rice, wheat, sugar, and kerosene (cooking fuel) from the government fair price shops. Moreover, 90% of the women with iron deficiency had access to and utilized the PDS services (GAIN baseline report, 2016, unpublished). The introduction of DFS in the PDS would, therefore, ensure iron intake of at least 30-40% of Dietary Reference Intakes (DRI), in more than 80% of the most vulnerable population. Considering acceptability based on sensory trials, DFS would be consumed by most of this population. However, the effective coverage of DFS through PDS depends on consumer uptake and utilization of DFS, which may vary across settings. Since DFS is a new product and most of the population is unaware of its health potential, there is no existing demand for the product. DFS interventions would have to create a demand for DFS in order to be scaled-up and this means changing the behavior of consumers who prefer to buy other salts easily available in the open market at relatively affordable prices. Hence, the key to ensuring the acceptability of DFS and use at-scale in the community lies in the health awareness levels, and demand creation for fortified products in the community. DFS by nature is organoleptically slightly different from the regular salt and perceived notions of high-quality salt is a critical barrier. Thus, in some situations, consumer illiteracy and consumer preferences may offset the expected increase in demand by providing subsidies. Increase in awareness of DFS and entry of DFS in the private sector may create a demand for the product, eventually transforming into a pull system. In certain geographies, knowledge and awareness levels are low to begin with and slow to show improvement. In such situations, mandatory fortification for public health reasons may be justified; especially when no adverse effects are reported, the purchasing price is unaffected, and the incremental industry cost of fortification is meager. Until then, consumers having alternative choices to purchase their salt in the open market need to be informed and convinced about the health benefits of the sustained use of DFS.
A favorable policy environment, partnership with the salt industry, and consumer demand for DFS are the foundations of the scale-up of DFS. Policies such as mandatory inclusion of DFS in food and nutrition programs can be a starting point to create demand beginning with institutional markets such as the PDS and ICDS. Salt production in India is purely in the private domain, and therefore, the cost of fortification would be influenced by the market. Market policies such as tax rebates for pre-mix and DFS manufacturers could support the development of the market for DFS and help to keep prices low. Also, the potentially high coverage of the intervention due to the integration of DFS with the public distribution system and choice of a universally consumed food vehicle (salt) – resulting in enhanced nutritional outcomes – is expected to increase the cost-effectiveness of the intervention in the long run. Partnership with the salt industry as well as infrastructure and equipment for iron premix production are essential organizational elements for a full scale-up. The investments and alliances with the industry could be sustainable only if the demand for DFS catches up the supply potential. Thus, consumer awareness and demand would be the most critical driver deciding the scaling-up potential of this promising intervention. An essential consideration for scaling-up is the cost-effectiveness of an intervention. DFS has a high benefit:cost ratio of 6:1 that rises to 36:1 when discounted future benefits due to cognitive improvements are included33 The unit costs for the intervention is slightly higher than other studies, yet much less than supplementation programs.34 However, considering the high benefit:cost ratio, economies of scale and efficient methods of DFS distribution are expected to further reduce the costs.
This case study has sought to understand the critical contextual factors for fortification inventions such as enabling policy environment and political leadership; appropriate technology, institutional infrastructure, and market incentives for the private sector; and consumer awareness and acceptance of the product. To our knowledge, there are very few case studies that have evaluated the integrated role of these factors in successful scaling-up of fortification interventions. Most notably, there has been inadequate attention given to the role of the private sector as a source of innovative financing for global health nutrition. Integration with other public food and nutrition programs, multi-sectoral partnerships for financing and implementation, addressing contextual factors influencing scale-up, and consumer literacy on fortification are essential considerations for large-scale food fortification interventions. Our case study highlights the need for further research in understanding the approaches and pathways of scale-up models and contextual factors in scaling-up fortification programs. Our paper brings out the complexities of implementing a multi-partnership fortification program on a large-scale and provides learnings to inform future program and research designs in scaling-up fortification interventions; especially using the public sector channels. Our research has high local and national relevance, and also significant implications for global nutrition programming directed at the reduction of micronutrient deficiencies. Primarily, we propose and demonstrate the integration of DFS and food security interventions targeted to vulnerable populations, as an efficient way to address iron deficiency anemia, when scalability considerations are adequately met.
Limitations of the study
While we understand that the scalability assessment of the project’s model can best be done externally, in our opinion the preparation of the case study to document the model, the processes, and implementation experiences and challenges is best done by an insider; someone closely and continuously involved in the scale-up process. Our findings are limited to our implementation experiences, and the same model may have different results in a different setting. Further follow-up on the sustainability of the intervention is also needed. The cost considerations for scaling-up DFS need further exploration involving a full costing analysis that was beyond the scope of this case study.
CONCLUSION AND POLICY IMPLICATIONS
Introducing fortified food and food products in existing nutrition and food security schemes can accelerate the scaling-up of fortification interventions and reduction of micronutrient deficiencies. Several contextual factors critical to scaling-up, from both the supply and demand perspectives, should be considered before replication and expansion. Public policies and food regulations promoting fortification are key factors in ensuring the scale-up of fortified foods. However, the nature of the fortified product, health literacy of the population, operational efficiencies of the distribution mechanism, sustainable financing, and consumer choices, food behaviors, and taste influence the effectiveness of fortification interventions and should, therefore, be appropriately evaluated and addressed. Consumer behavior and acceptability of fortified foods could be altered by using the ‘nudge factor’ by making fortified foods easily and readily available at an affordable price. At the same time, consumer preferences and tastes should be considered while developing new fortified products. Demand creation through consumer awareness and promotion of fortified foods is urgently needed if food fortification were to be a global health success. Mass fortification should be encouraged through public-private partnerships with the food industry voluntarily fortifying their products until such a time that mandatory fortification is feasible. Partnership with the private sector (premix producers and salt industry), to mobilize private investments, along with creating sustained consumer demand, is essential to ensure sustainability.
Acknowledgements
Tata Trusts - The India Nutrition Initiative, and International Development Research Centre and Global Affairs Canada through the Canadian International Food Security Research Fund, partially funded the field intervention with major funding provided by the Government of Uttar Pradesh, India.
Funding
None.
Competing interests
The authors completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available upon request from the corresponding author) and declare no conflicts of interest.